Diagnosing and Managing Seborrheic Dermatitis in the African American Population
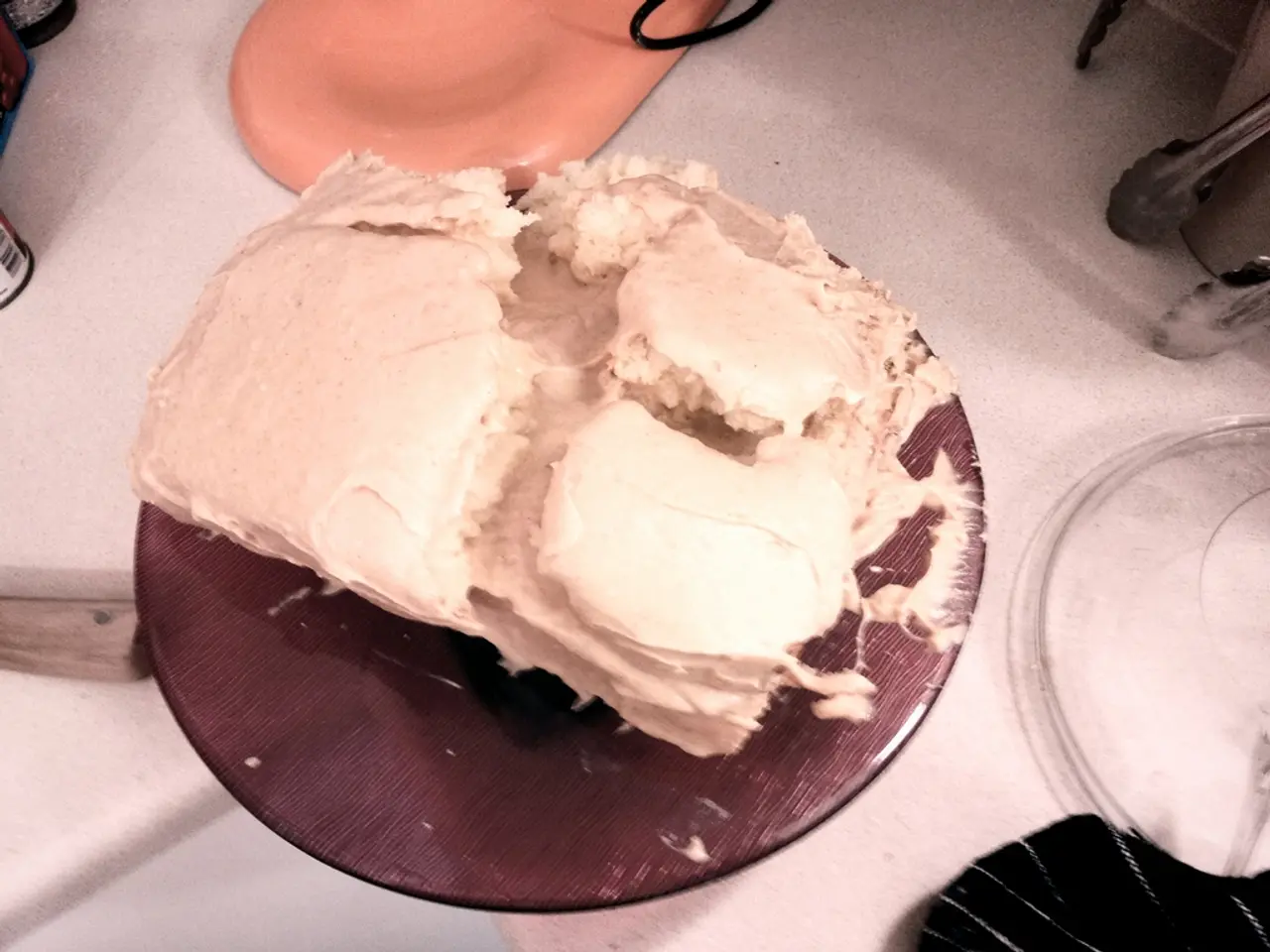
Seborrheic dermatitis is a common inflammatory skin disorder that affects people of all ages and skin types. It typically presents as red, flaky, scaly, greasy, and sometimes itchy patches affecting areas rich in oil-producing glands such as the scalp, face, chest, and other sebaceous regions[1][2].
In people with darker skin tones, the patterns of seborrheic dermatitis are mostly similar, but redness may be less visually apparent and the affected areas can show more prominent scaling, hyperpigmentation, or post-inflammatory pigmentary changes rather than classic bright redness[3]. The lesions might appear as grayish or darker patches rather than bright red, with inflammation visible on palpation rather than just inspection[3].
Recommended treatments primarily include topical antifungal agents such as ketoconazole or ciclopirox creams or shampoos to reduce Malassezia yeast, which is implicated in the condition[2][3]. These are often combined with anti-inflammatory agents—typically mild topical corticosteroids or calcineurin inhibitors—to reduce inflammation and itch[2].
For dark skin, particular care is advised due to the risk of post-inflammatory hyperpigmentation or hypopigmentation from both the disease and treatment. Using gentle anti-inflammatory creams, avoiding potent steroids long-term, and monitoring pigment changes are recommended[3]. Regular use of medicated shampoos (ketoconazole, selenium sulfide, or zinc pyrithione) for scalp involvement is common. Over-the-counter options and prescription treatments should be personalized to minimize irritation and pigmentary side effects especially in darker skin tones[3].
Research from 2015 lists coal tar shampoo, tea tree oil shampoo, antifungal creams, and mineral oil or petroleum jelly as over-the-counter remedies for seborrheic dermatitis[4]. Researchers from 2019 found that Black people preferred to use ointment or oil preparations to treat their seborrheic dermatitis[4].
A doctor may diagnose seborrheic dermatitis based on the location and appearance of the rash, or by taking a skin biopsy. Certain conditions or outside factors can increase a person's chances of developing seborrheic dermatitis, such as increased sebaceous gland activity, conditions that weaken the immune system, certain medications, stress, and cold, dry weather[5].
Certain lifestyle changes, such as washing hair frequently, reducing the use of pomades or hair oils, applying hair emollients to the hair shaft only, keeping track of triggers, reducing stress levels, and avoiding cold, dry weather, can help reduce the chances of a seborrheic dermatitis flare-up[5].
Cradle cap, a form of seborrheic dermatitis, can occur in infants and can develop on the scalp and groin area. Resources like the Skin of Color Society's "Find a Doctor" tool can help connect people with doctors who have experience in treating skin issues in skin of color.
- The redness in seborrheic dermatitis might be less apparent in people with darker skin tones, but they may instead experience more noticeable scaling, hyperpigmentation, or post-inflammatory pigmentary changes.
- For dark skin, it is recommended to use gentle anti-inflammatory creams and to avoid potent steroids long-term to minimize the risk of post-inflammatory hyperpigmentation or hypopigmentation from both the disease and treatment.
- Research from 2015 suggests that coal tar shampoo, tea tree oil shampoo, antifungal creams, and mineral oil or petroleum jelly can be over-the-counter remedies for seborrheic dermatitis.
- A medical entity called the Skin of Color Society provides a tool to help people find doctors who have experience in treating skin issues in skin of color, which can be particularly useful for managing conditions like seborrheic dermatitis.